Articles
- Page Path
- HOME > Epidemiol Health > Volume 41; 2019 > Article
-
Original Article
Geospatial analysis and epidemiological aspects of human infections with Blastocystis hominis in Mazandaran Province, northern Iran -
Shabnam Asfaram1,2
 , Ahmad Daryani1,3
, Ahmad Daryani1,3 , Shahabeddin Sarvi1,3
, Shahabeddin Sarvi1,3 , Abdol Sattar Pagheh1,2
, Abdol Sattar Pagheh1,2 , Seyed Abdollah Hosseini1,2
, Seyed Abdollah Hosseini1,2 , Reza Saberi1,2
, Reza Saberi1,2 , Seyede Mahboobeh Hoseiny4
, Seyede Mahboobeh Hoseiny4 , Masoud Soosaraei1,2
, Masoud Soosaraei1,2 , Mehdi Sharif1,3
, Mehdi Sharif1,3
-
Epidemiol Health 2019;41:e2019009.
DOI: https://doi.org/10.4178/epih.e2019009
Published online: March 28, 2019
1Toxoplasmosis Research Center, Mazandaran University of Medical Sciences, Sari, Iran
2Student Research Committee, Mazandaran University of Medical Sciences, Sari, Iran
3Department of Parasitology, School of Medicine, Mazandaran University of Medical Science, Sari, Iran
4Geographic Information System Research Center, Mazandaran University of Medical Science, Sari, Iran
- Correspondence: Mehdi Sharif Toxoplasmosis Research Center, Mazandaran University of Medical Sciences, P. O. Box 48168-95475, Sari, Iran E-mail: msharifmahdi@yahoo.com
• Received: February 8, 2019 • Accepted: March 28, 2019
©2019, Korean Society of Epidemiology
This is an open-access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
-
OBJECTIVES
- Blastocystis hominis is a very common large intestinal protozoan with global prevalence in humans and non-human hosts. No precise statistics exist regarding the geographical distribution of Blastocystis that would enable the identification of high-risk communities. Therefore, the current research aimed to characterize the spatial patterns and demographic factors associated with B. hominis occurrence in northern Iran.
-
METHODS
- The current study was performed among 4,788 individuals referred to health centers in Mazandaran Province, from whom stool samples were obtained. Socio-demographic data were gathered using a questionnaire. Samples were examined by a direct wet mount, the formalin-ethyl acetate concentration technique, and trichrome staining. Moran local indicators of spatial association and a geographically weighted regression model were utilized to analyze the results.
-
RESULTS
- Generally, the infection rate of Blastocystis parasites was 5.2%, and was considerably higher in the age group of 10-14 years (10.6%) than in other age groups (p=0.005). Our data showed important associations between the occurrence of B. hominis and age, residence, job, contact with domestic animals, anti-parasitic drug consumption, and elevation above sea level (p<0.001).
-
CONCLUSIONS
- The current study characterized for the first time the infection rate and risk of B. hominis in the north of Iran, and produced a prediction map. It is expected that this map will help policymakers to plan and implement preventive measures in high-risk areas and to manage already-infected patients.
- Blastocystis hominis is the most common intestinal protozoan, with a wide geographic distribution that has unclear clinical significance [1]. It is a morphologically variable protozoan that can exist in granular, vacuolar, amoeboid, and cystic forms. Vacuolar forms are most often observed under microscopic examination. The amoeboid forms are considered pathogenic and responsible for the manifestation of clinical symptoms, including various intestinal conditions. With symptoms similar to those of irritable bowel syndrome, transmission of Blastocystis occurs by the fecaloral route through the consumption of contaminated water or food [2,3]. Although this parasite can be asymptomatic, in immunocompromised patients it can function as an opportunistic pathogen and cause gastrointestinal disorders [4]. Blastocystis spp. are considered to be pathogenic whenever more than 5 parasites are detected in each microscopic field without the presence of other organisms [4,5]. Because of the variable size of the parasite and its similarity to fat drops, yeast, and white blood cells, it has been recommended to apply several diagnostic tests to detect Blastocystis in stool specimens [6]. The prevalence of Blastocystis infection varies from 1.6% to 16.0% in developed countries, such as Singapore and Japan [7,8] and can reach 60.0% in developing countries including Senegal, Cuba, Brazil, and Argentina [9-12]. In Iran, the total prevalence of B. hominis in the total population has been estimated to be 3.0% [13]. Because of the high infection rate, data collection and analysis are essential for identifying high-risk locations, factors related to incidence, and control strategies for Blastocystis. The use of a geographic information system is a strategy that could enable a more accurate evaluation of the distribution of the illness in a high-incidence community and improvements in approaches to avoid infection spread. Therefore, using this powerful tool, along with a risk factor questionnaire, constitutes a true environmental health approach [14]. The current study was performed to study the prevalence and geospatial distribution of Blastocystis among the total population in Mazandaran Province (in northern Iran) and to identify factors associated with the occurrence of B. hominis.
INTRODUCTION
- Study area
- This cross-sectional study was performed in Mazandaran Province, which is located in northern Iran (35°47ʹ to 36°35ʹN, 50°34ʹ to 54°10ʹE). This province consists of 19 cities and a population of 3,073,943 people. This area has a subtropical climate with an average annual relative humidity of 83%, an average temperature of 18°C, and rainfall occurrence during all four seasons of the year [15].
- Ethics Statement
- First, the study protocol was evaluated and approved by the Medical Research Ethics Committee of Mazandaran University of Medical Sciences, Sari, Iran. Informed permission was then obtained from all participants.
- Sample collection
- The participants of the current study included 4,788 individuals referred to health centers in Mazandaran Province from January to December 2016. A questionnaire was prepared on the basis of socio-demographic data, and assessed possible parameters related to Blastocystis prevalence, including age, sex, site of residence, type of consumed water, job, education, contact with domestic animals, season, and anti-parasitic drug use.
- Fresh stool specimens were collected after subjects agreed to participate in the study and completed the questionnaire. The samples were kept in a clean plastic container, fixed in polyvinyl alcohol, and then transferred to the Parasitology Laboratory of Mazandaran University of Medical Sciences.
- Stool examination
- All samples were tested with normal saline (0.85% NaCl) for the presence of trophozoites and Lugol iodine staining for the recognition of Blastocystis cysts under an optical microscope with × 40 objective magnification. Then, formalin-ether and trichrome staining methods [16] were used to visualize all specimens.
- Geographical data
- In our research, data on elevation above sea level (< 500 m, 500- 1,000 m, and > 1,000 m) and distance from the sea (< 10 km, 10- 20 km, and > 20 km) were acquired from Google Earth version 16 (https://www.google.com/earth/). Ecological data (such as temperature, rain, moisture, elevation above sea level, and distance from the sea) were acquired from the Mazandaran Metrological Institute.
- Statistical analysis
- The outcomes of the study were analyzed using SPSS version 16.0 (SPSS Inc., Chicago, IL, USA). Local indicators of spatial association were used to characterize the distribution of B. hominis and potential risk factors in various areas of the province. Additionally, geographically weighted regression (GWR) was applied to examine the geographical relationships between the occurrence of Blastocystis and related main variables, including temperature and precipitation.
MATERIALS AND METHODS
- Of the 4,788 individuals referred to health centers, 2,579 (53.9%) were male and 2,209 (46.1%) were female. The average age was 32.39± 17.75 years (range, 1-77 years).
- In total, 247 (5.2%) individuals were positive for B. hominis. The outcomes demonstrated statistically significant relationships between the prevalence of B. hominis and age, occupation, residence, contact with domestic animals, and anti-parasitic drug consumption (p< 0.05) (Table 1).
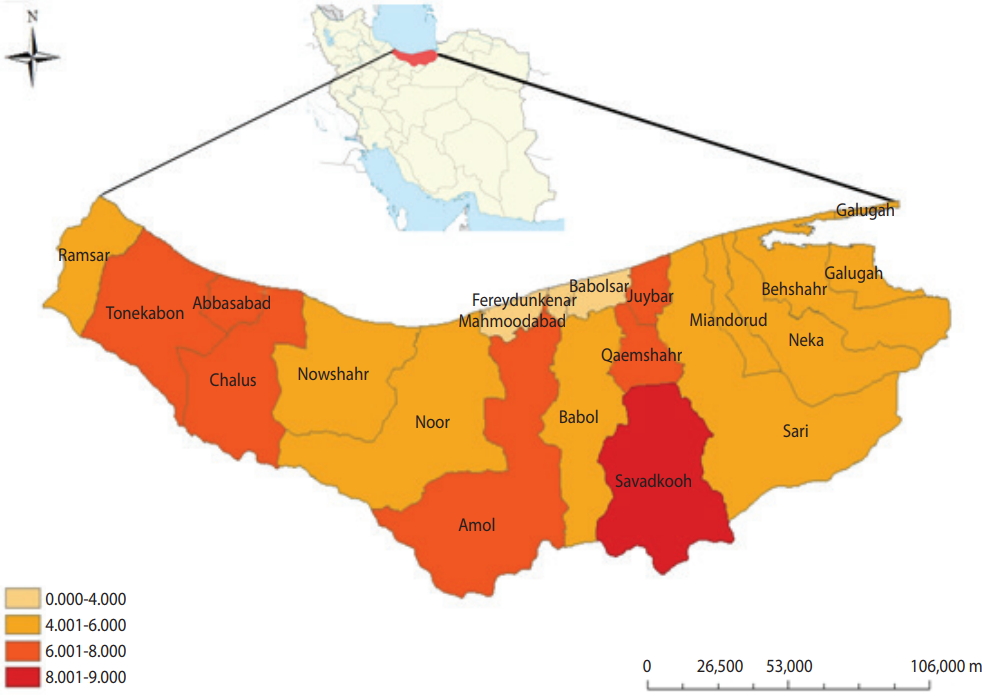
- Based on the outcomes of this research, the prevalence rates of Blastocystis according to elevation above sea level was as follows: < 500 m, 4.3% (74 of 1,710); 500-1,000 m, 5.4% (162 of 2,954); and > 1,000 m, 8.9% (11 of 124). Of the meteorological risk factors, only elevation above sea level of > 1,000 m showed a significant difference from sea level (p< 0.05). Mapping the infection rate of B. hominis in Mazandaran Province showed that the Savadkooh (8.9%) and Babolsar (1.9%) districts had the maximum and minimum occurrence level of B. hominis, respectively (Figure 1).
RESULTS
- Blastocystis is the most common parasite worldwide and has a global distribution. During recent years, despite improvements in health services, the outcomes of epidemiological studies in numerous parts of the world have indicated that Blastocystis infection remains an important health problem in tropical and subtropical areas, particularly in developing countries [17].
- Several investigations in Iran have revealed infection rates of 2.4% to 54.5% [18-21]. A meta-analysis in Iran showed an infection rate of 3.0% in the overall population [13]. It seems that differences in the prevalence of B. hominis infection may be caused by diverse parameters, such as sample size, type of consumed water, inconsistent laboratory approaches, and ecological parameters.
- In the current study, the highest prevalence rate of B. hominis was reported in individuals aged 10-14 (10.6%). We observed a significant relationship between B. hominis infection and age (p= 0.005), which is in accordance with research performed in Bangladesh [22] and Brazil [23]. Some studies have reported a high prevalence of this infection among all age groups [24,25], possibly due to behavioral patterns and high levels of activity.
- The prevalence of B. hominis demonstrated significant variation by area (p< 0.001), which is in accordance with studies conducted in South Khorasan of Iran [26] and Turkey [27]. In rural and urban regions, the incidence of B. hominis was 7.0% and 3.4%, respectively; the higher rate in rural regions can be explained as the result of poor sanitation, lack of healthy drinking water reservoirs, more contact with the soil, environmental contamination with the cystic form, a large number of households, and geographical factors.
- In the current study, 6.2% of the infected subjects had experienced contact with animals (p= 0.001). Several studies have found animal ownership to be a risk factor for Blastocystis infection [28- 32].
- Our investigation showed that there was a significant relationship between taking anti-parasitic drugs and infection with B. hominis. However, 3.2% and 5.7% of subjects with and without a history of anti-parasitic drug consumption were infected with B. hominis, respectively (p= 0.001). Similar to several other studies, our findings showed that consumption of anti-parasitic drugs may be an important reason for the reduction in parasitic infections in recent years.
- In this study, there was a significant relationship between certain jobs and infection with B. hominis (p< 0.001). The prevalence rate of B. hominis in farmers (8.7%) was higher than in people with other occupations. Our result is in accordance with the research performed by Banai in Ghazvin Province of Iran [33]. The high prevalence of infection in agriculturists may be because of their high exposure to manure and human excrement in the soil [34].
- In this research, similar to other studies, no meaningful relationships were found between the prevalence of Blastocystis and sex (p= 0.795), type of consumed water (p= 0.857), education level (p= 0.964), or season (p= 0.399) [35-39].
- Despite awareness of the impacts of environmental factors on B. hominis, few attempts have been made to map the distribution of this parasite in relation to particular ecological parameters in Iran. Based on the map prepared in this research, Savadkooh district had the maximum prevalence of B. hominis. This city is situated in the south of Mazandaran Province, in the northern Alborz Mountains, at a height of 1,000 m. The high rate of Blastocystis in Savadkooh district seems to be because of its geographical location, contact with animals, agriculture activities, and the presence of many villages in this region.
- Furthermore, the elevation of Savadkooh district above sea level was estimated to be more favorable for cyst persistence [40,41]. The concordance between higher prevalence and elevation could be explained by the fact that cysts are viable for longer in cold climates [41]. Additionally, the transportation of livestock from the plains to mountainous areas in the warm season may influence parasite transmission to different regions. In this study, GWR was applied to examine the geographical relationship of the prevalence of B. hominis with several significant factors, including precipitation, temperature, and livestock. The outcomes indicate that 65% and 60% of the prevalence of Blastocystis could be explained by contact with domestic animals and rainfall, respectively. This fact highlights the significant impact of these 2 main factors.
- Based on our research, the prevalence of Blastocystis in mountainous areas may be high because of the more widespread use of unfiltered water sources, high levels of husbandry and agriculture, and lack of good hygiene practices. This geospatial study demonstrated that living in regions with low elevation and converting traditional livestock to industrial livestock could effectively decrease Blastocystis infections in different districts in Mazandaran Province. Therefore, the populations living in areas with suitable environmental factors for the parasite are potentially at risk for Blastocystis infection.
DISCUSSION
ACKNOWLEDGEMENTS
Figure 1.Spatial distribution of Blastocystis hominis among the general population in Mazandaran Province. The light-colored areas had the lowest Blastocystis rates, while the dark areas had the highest rates by ArcGIS 9.2 (https://support.esri.com/en/).


Table 1.Frequency of Blastocystis hominis in Mazandaran Province by demographic data and risk factors
- 1. Alfellani MA, Stensvold CR, Vidal-Lapiedra A, Onuoha ES, Fagbenro-Beyioku AF, Clark CG. Variable geographic distribution of Blastocystis subtypes and its potential implications. Acta Trop 2013;126:11-18.ArticlePubMed
- 2. Eida AM, Eida MM. Identification of Blastocystis hominis in patients with irritable bowel syndrome using microscopy and culture compared to PCR. Parasitol United J 2008;1:87-92.
- 3. Woodhall D, Jones JL, Cantey PT, Wilkins PP, Montgomery SP. Neglected parasitic infections: what every family physician needs to know. Am Fam Physician 2014;89:803-811.PubMed
- 4. Stensvold CR, Nielsen HV, Mølbak K, Smith HV. Pursuing the clinical significance of Blastocystis–diagnostic limitations. Trends Parasitol 2009;25:23-29.ArticlePubMed
- 5. Stenzel DJ, Boreham PF. Blastocystis hominis revisited. Clin Microbiol Rev 1996;9:563-584.ArticlePubMedPMC
- 6. Stensvold CR, Smith HV, Nagel R, Olsen KE, Traub RJ. Eradication of Blastocystis carriage with anti-microbials: reality or delusion? J Clin Gastroenterol 2010;44:85-90.ArticlePubMed
- 7. Wong KH, Ng GC, Lin RT, Yoshikawa H, Taylor MB, Tan KS. Predominance of subtype 3 among Blastocystis isolates from a major hospital in Singapore. Parasitol Res 2008;102:663-670.ArticlePubMedPDF
- 8. Hirata T, Nakamura H, Kinjo N, Hokama A, Kinjo F, Yamane N, et al. Prevalence of Blastocystis hominis and Strongyloides stercoralis infection in Okinawa, Japan. Parasitol Res 2007;101:1717-1719.ArticlePubMedPDF
- 9. El Safadi D, Gaayeb L, Meloni D, Cian A, Poirier P, Wawrzyniak I, et al. Children of Senegal River Basin show the highest prevalence of Blastocystis sp. ever observed worldwide. BMC Infect Dis 2014;14:164.ArticlePubMedPMC
- 10. Escobedo AA, Cañete R, Núñez FA. Intestinal protozoan and helminth infections in the Municipality San Juan y Martínez, Pinar del Río, Cuba. Trop Doct 2007;37:236-238.ArticlePubMed
- 11. Aguiar JI, Gonçalves AQ, Sodré FC, Pereira Sdos R, Bóia MN, de Lemos ER, et al. Intestinal protozoa and helminths among Terena Indians in the State of Mato Grosso do Sul: high prevalence of Blastocystis hominis. Rev Soc Bras Med Trop 2007;40:631-634.ArticlePubMedPDF
- 12. Basualdo JA, Córdoba MA, de Luca MM, Ciarmela ML, Pezzani BC, Grenovero MS, et al. Intestinal parasitoses and environmental factors in a rural population of Argentina, 2002-2003. Rev Inst Med Trop Sao Paulo 2007;49:251-255.ArticlePubMedPDF
- 13. Badparva E, Ezatpour B, Mahmoudvand H, Behzadifar M, Behzadifar M, Kheirandish F. Prevalence and genotype analysis of blastocystis hominis in Iran: a systematic review and meta-analysis. Arch Clin Infect Dis 2017;12:1-9.Article
- 14. Zhou XN, Lv S, Yang GJ, Kristensen TK, Bergquist NR, Utzinger J, et al. Spatial epidemiology in zoonotic parasitic diseases: insights gained at the 1st International Symposium on Geospatial Health in Lijiang, China 2007. Parasit Vectors 2009;2:10.ArticlePubMedPMC
- 15. Daryani A, Sharif M, Nasrolahei M, Khalilian A, Mohammadi A, Barzegar G. Epidemiological survey of the prevalence of intestinal parasites among schoolchildren in Sari, northern Iran. Trans R Soc Trop Med Hyg 2012;106:455-459.ArticlePubMedPDF
- 16. Garcia LS. Diagnostic medical parasitology. 5th ed. Santa Monica: American Society for Microbiology Press; 2007. p 57-101.
- 17. Ithoi I, Jali A, Mak JW, Wan Sulaiman WY, Mahmud R. Occurrence of Blastocystis in water of two rivers from recreational areas in Malaysia. J Parasitol Res 2011;2011:123916.ArticlePubMedPMCPDF
- 18. Haghighi A, Khorashad AS, Nazemalhosseini Mojarad E, Kazemi B, Rostami Nejad M, Rasti S. Frequency of enteric protozoan parasites among patients with gastrointestinal complaints in medical centers of Zahedan, Iran. Trans R Soc Trop Med Hyg 2009;103:452-454.ArticlePubMedPDF
- 19. Daryani A, Barmaki N, Ettehad GH, Sharif M, Nemati A, Ziaei H. A cross-sectional study of Blastocystis hominis in primary school children, Northwest Iran. Inter J Trop Med 2006;1:53-57.
- 20. Zali MR, Mehr AJ, Rezaian M, Meamar AR, Vaziri S, Mohraz M. Prevalence of intestinal parasitic pathogens among HIV-positive individuals in Iran. Jpn J Infect Dis 2004;57:268-270.ArticlePubMed
- 21. Heidari A, Rokni MB. Prevalence of intestinal parasites among children in day-care centers in Damghan-Iran. Iran J Public Health 2003;32:31-34.
- 22. Hossain MM, Ljungstrom I, Glass RI, Lundin L, Stoll BJ, Huldt G. Amoebiasis and giardiasis in Bangladesh: parasitological and serological studies. Trans R Soc Trop Med Hyg 1983;77:552-554.ArticlePubMedPDF
- 23. Braga LL, Lima AA, Sears CL, Newman RD, Wuhib T, Paiva CA, et al. Seroepidemiology of Entamoeba histolytica in a slum in northeastern Brazil. Am J Trop Med Hyg 1996;55:693-697.ArticlePubMed
- 24. Al-Harazi T, Ghani MK, Othman H. Prevalence of intestinal protozoan infections among Orang Asli schoolchildren in Pos Senderut, Pahang, Malaysia. J Egyp Soc Parasitol 2013;43:561-568.Article
- 25. Sukthana Y. Is Blastocystis hominis a human pathogenic protozoan. J Trop Med Parasitol 2001;24:16-22.
- 26. Taheri F, Namakin K, Zarban A, Sharifzadeh G. Intestinal parasitic infection among school children in South Khorasan Province, Iran. J Res Health Sci 2011;11:45-50.PubMed
- 27. Aksoy U, Akisü C, Bayram-Delibaş S, Ozkoç S, Sahin S, Usluca S. Demographic status and prevalence of intestinal parasitic infections in schoolchildren in Izmir, Turkey. Turk J Pediatr 2007;49:278-282.PubMed
- 28. Doyle PW, Helgason MM, Mathias RG, Proctor EM. Epidemiology and pathogenicity of Blastocystis hominis. J Clin Microbiol 1990;28:116-121.ArticlePubMedPMC
- 29. Rajah Salim H, Suresh Kumar G, Vellayan S, Mak JW, Khairul Anuar A, Init I, et al. Blastocystis in animal handlers. Parasitol Res 1999;85:1032-1033.ArticlePubMedPDF
- 30. Li LH, Zhou XN, Du ZW, Wang XZ, Wang LB, Jiang JY, et al. Molecular epidemiology of human Blastocystis in a village in Yunnan province, China. Parasitol Int 2007;56:281-286.ArticlePubMed
- 31. Stensvold CR, Suresh GK, Tan KS, Thompson RC, Traub RJ, Viscogliosi E, et al. Terminology for Blastocystis subtypes–a consensus. Trends Parasitol 2007;23:93-96.ArticlePubMed
- 32. Yoshikawa H, Wu Z, Pandey K, Pandey BD, Sherchand JB, Yanagi T, et al. Molecular characterization of Blastocystis isolates from children and rhesus monkeys in Kathmandu, Nepal. Vet Parasitol 2009;160:295-300.ArticlePubMed
- 33. Banai F. A survey of the prevalence of intestinal parasites in the city of Ghazvin during 2001-2002 [dissertation]. Tehran: Tehran University; 2002. (Persian).
- 34. Shahabi S. Epidemiological study of intestinal parasites among primary school students in Shahryar in 1993. Pejouhesh 2000;24:133-139 (Persian).
- 35. Cegielski JP, Msengi AE, Dukes CS, Mbise R, Redding-Lallinger R, Minjas JN, et al. Intestinal parasites and HIV infection in Tanzanian children with chronic diarrhea. AIDS 1993;7:213-221.ArticlePubMed
- 36. Yaicharoen R, Ngrenngarmlert W, Wongjindanon N, Sripochang S, Kiatfuengfoo R. Infection of Blastocystis hominis in primary schoolchildren from Nakhon Pathom province, Thailand. Trop Biomed 2006;23:117-122.PubMed
- 37. Shahbazi AE, Rezaeian M, Eshraghian MR, Mohebali M, Rokni MB, Sharifdini M, et al. he prevalence of human intestinal parasites in rural areas of Saveh, Markazi Province, Iran. J Fasa Univ Med Sci 2014;4:177-184 (Persian).
- 38. EL-Marhoumy SM, EL-Nouby KA, Shoheib ZS, Salama AM. Prevalence and diagnostic approach for a neglected protozoon Blastocystis hominis. Asian Pac J Trop Dis 2015;5:51-59.Article
- 39. Alver O, Töre O. The prevalence and distribution of intestinal parasites detected by the Uludag University Medical School. Turkiye Parazitol Derg 2006;30:296-301 (Turkish).PubMed
- 40. Leelayoova S, Siripattanapipong S, Thathaisong U, Naaglor T, Taamasri P, Piyaraj P, et al. Drinking water: a possible source of Blastocystis spp. subtype 1 infection in schoolchildren of a rural community in central Thailand. Am J Trop Med Hyg 2008;79:401-406.ArticlePubMed
- 41. Schmidt GD, Roberts LS, Janovy Jr J. Foundation of parasitology. 6th ed. New York: Mcgraw-Hill; 2000. p 347-410.
REFERENCES
Figure & Data
References
Citations
Citations to this article as recorded by 

- A 11-year-old boy with Blastocystis hominis infection, presents as immune thrombocytopenia
Fajuan Tang, Dongqiong Xiao, Lin Chen, Xihong Li, Lina Qiao
Thrombosis Journal.2024;[Epub] CrossRef - Blastocystis colonization and associations with population parameters in Thai adults
Vasana Jinatham, Amara Yowang, Christen Rune Stensvold, Eleni Michalopoulou, Thanakrit Vichasilp, Picha Suwannahitatorn, Siam Popluechai, Anastasios D. Tsaousis, Eleni Gentekaki, Funda Dogruman-Al
PLOS Neglected Tropical Diseases.2024; 18(7): e0012292. CrossRef - Molecular epidemiology and subtyping of Blastocystis sp. and its subtypes in celiac patients; a case control study
Sara Soleimani Jevinani, Hanieh Mohammad Rahimi, Nastaran Asri, Mohammad Rostami-Nejad, Shokoufeh Ahmadipour, Hamed Mirjalali
Microbial Pathogenesis.2023; 179: 106086. CrossRef - Development and evaluation of a loop-mediated isothermal amplification (LAMP) technique for rapid, accurate, and specific detection of Blastocystis spp. in AIDS patients
Ebrahim Badparva, Amirreza Javadi Mamaghani, Farnaz Kheirandish, Farzad Ebrahimzadeh, Shirzad Fallahi
Infection.2022; 50(5): 1295. CrossRef - In vitro susceptibility of human Blastocystis subtypes to simeprevir
Shereen F. Mossallam, Salwa A.T. El- Mansoury, Mona M. Tolba, Asmaa A. Kohla, Safaa I. Khedr
Saudi Journal of Biological Sciences.2021; 28(4): 2491. CrossRef - Epidemiology and subtype distribution of Blastocystis in humans: A review
Supaluk Popruk, Davin Edric V. Adao, Windell L. Rivera
Infection, Genetics and Evolution.2021; 95: 105085. CrossRef - The Coexistence of Blastocystis spp. in Humans, Animals and Environmental Sources from 2010–2021 in Asia
Adedolapo Aminat Rauff-Adedotun, Farah Haziqah Meor Termizi, Nurshafarina Shaari, Ii Li Lee
Biology.2021; 10(10): 990. CrossRef - Prevalence and subtype identification of Blastocystis isolated from human in Shiraz city, southern Iran
Lida Haghighi, Seyed Emad Talebnia, Fattaneh Mikaeili, Qasem Asgari, Fatemeh Gholizadeh, Kamiar Zomorodian
Clinical Epidemiology and Global Health.2020; 8(3): 840. CrossRef - Improving Hashimoto’s thyroiditis by eradicating Blastocystis hominis: Relation to IL-17
Hanaa Tarek El-Zawawy, Huda Fahmy Farag, Mona Mohamed Tolba, Hanaa Abdalbasit Abdalsamea
Therapeutic Advances in Endocrinology and Metabolism.2020; 11: 204201882090701. CrossRef - Comparing spatio‐temporal distribution of the most common human parasitic infections in Iran over two periods 2007 to 2012 and 2013 to 2018: A systematic quantitative literature review
Behzad Kiani, Amene Raouf Rahmati, Robert Bergquist, Elham Moghaddas
The International Journal of Health Planning and Management.2020; 35(5): 1023. CrossRef

 KSE
KSE
 PubReader
PubReader ePub Link
ePub Link Cite
Cite