Articles
- Page Path
- HOME > Epidemiol Health > Volume 44; 2022 > Article
-
Original Article
Long working hours and the risk of hypothyroidism in healthy Korean workers: a cohort study -
Yesung Lee1
 , Woncheol Lee1
, Woncheol Lee1 , Hyoung-Ryoul Kim2
, Hyoung-Ryoul Kim2
-
Epidemiol Health 2022;44:e2022104.
DOI: https://doi.org/10.4178/epih.e2022104
Published online: November 8, 2022
1Department of Occupational and Environmental Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
2Department of Occupational and Environmental Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea
- Correspondence: Hyoung-Ryoul Kim, Department of Occupational and Environmental Medicine, College of Medicine, The Catholic University of Korea, 222 Banpo-daero, Seocho-gu, Seoul 06591, Korea, E-mail: cyclor@catholic.ac.kr
© 2022, Korean Society of Epidemiology
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
-
OBJECTIVES
- Long working hours have been reported to cause various health problems, but are currently practiced in many countries. Building upon a previous cross-sectional study, the authors aimed to elucidate the causal relationship between long working hours and hypothyroidism through a longitudinal study.
-
METHODS
- Data were collected at baseline from 45,259 participants without thyroid disease and with consistent weekly working hours (36–40, 41–52, 53–60, and >60 hours) during the follow-up period. Hypothyroidism was defined using the reference limits of serum thyroid-stimulating hormone and free thyroxine levels. By estimating hazard ratios (HRs) and 95% confidence intervals (CIs) using Cox proportional hazards regression analysis, the risk of incident hypothyroidism was evaluated with 36–40 hours of work per week as the reference.
-
RESULTS
- During 138,261.7 person-years of follow-up, 2,914 participants developed hypothyroidism (incidence density, 2.11/102 person-years). The multivariable-adjusted HRs of incident hypothyroidism for 41–52 hours, 53–60 hours, and >60 hours of work per week were 1.13 (95% CI, 1.03 to 1.24), 2.53 (95% CI, 2.17 to 2.95), and 2.57 (95% CI, 2.09 to 3.15), respectively. In dose-response analyses, long working hours had an approximately linear relationship with hypothyroidism incidence. The risk of incident hypothyroidism in those who worked 53–60 hours and >60 hours per week compared with the reference group was significantly higher among the older age group (≥36 years, stratified by median age), men, and daytime workers.
-
CONCLUSIONS
- This large-scale cohort study demonstrated the association between long working hours and an increased risk of incident hypothyroidism with a dose-response relationship.
- Occupational factors, such as long working hours, have been recognized as significant issues adversely affecting workers’ health [1–3]. In addition to threatening the health of workers, long working hours also reduce work efficiency, which can have a negative impact on an entire industry [4]. Nevertheless, there are many countries where long working hours are practiced. According to a report from the Organization for Economic Cooperation and Development (OECD) in 2020, the average annual hours actually worked was almost 2,000 hours in Colombia, Mexico, Costa Rica, and Korea, whereas the average of total OECD member countries was 1,687 hours [5]. Previous studies have shown that long working hours were associated with cerebro-cardiovascular disease [6], hypertension [7], diabetes mellitus (DM) [8], and obesity [9]. Furthermore, a recent cross-sectional study conducted in Korea reported that long working hours were associated with hypothyroidism [10].
- According to the Korea National Health and Nutrition Examination Survey (KNHANES VI) from 2013 to 2015, the prevalence of hypothyroidism was 3.8% [11]. Hypothyroidism is a globally common disease [12], which can contribute to cardiovascular disease, cognitive impairment, and chronic kidney disease [13,14]. As the importance of preventing hypothyroidism increases, epidemiological studies of hypothyroidism have reported occupational risk factors, such as shift work [15,16]. Moreover, a recent study using KNHANES VI data demonstrated that hypothyroidism was more prevalent in individuals who worked long hours [10]. However, because of the cross-sectional nature of that study, there was a limitation in elucidating the temporal relationship.
- Therefore, we aimed to conduct a longitudinal study to evaluate the causal relationship between long working hours and hypothyroidism by using data from the Kangbuk Samsung Health Study.
INTRODUCTION
- Study population
- The Kangbuk Samsung Health Study is a cohort study of Koreans aged at least 18 years who underwent annual or biennial comprehensive health screening examinations at the Kangbuk Samsung Hospital Total Healthcare Center in Seoul and Suwon, Korea [17]. Most of the examinees were employees of various companies and local governmental organizations and their spouses. In Korea, the Occupational Safety and Health Act requires annual or biennial health medical examinations to be provided to all employees for free. Other participants underwent health medical check-ups voluntarily at the healthcare center.
- Our study included a total of 218,904 participants who underwent health examinations from January 1, 2012 to December 31 2017, and had experienced at least one other screening exam before December 31, 2018. First, we excluded 83,598 participants who had any of the following conditions at baseline (Figure 1): missing data on thyroid function tests or working hours, history of malignancy, history of thyroid disease or medication use for thyroid disease, abnormal thyroid findings on ultrasonography, hypothyroidism or hyperthyroidism at baseline, surgical history of the thyroid, and working less than 36 hours per week. Second, among the potential participants (135,306 workers), we further excluded 90,047 participants whose category of working hours changed during the follow-up period because of fluctuations in their working hours per week. Finally, 45,259 participants were eligible for the study at baseline.
- Measurements
- All examinations were conducted at the Kangbuk Samsung Hospital Total Healthcare Screening Center in Seoul and Suwon. At each visit, information was collected on demographic characteristics, working characteristics, smoking status, alcohol consumption, medical history, and medication use using standardized, self-administered questionnaires [17]. Smoking status was categorized as non-current and current smokers. For alcohol consumption, heavy drinking was categorized as ≥30 g/day for men and ≥20 g/day for women. Cardiovascular disease was defined as a self-reported history of cardiovascular disease, or current use of medications for cardiovascular disease. On the day of the health examination, a trained nurse checked the questionnaire for blanks, and during the last stage of the health examination, a trained doctor double-checked the questionnaire for errors or blanks while conducting a face-to-face interview with the examinee.
- Working hours were assessed using the following question: “How many hours did you work in a week on average in your job for the past year, including overtime?” According to the Labor Standards Act of Korea, the working hours of adults should not exceed 40 hours per week except for break time (although 12 additional working hours per week are permitted with employees’ consent). This does not apply to workplaces with fewer than 5 employees, and workers in exceptional industries such as transportation services and health care services are permitted to work more than 52 hours per week. Meanwhile, if a person works more than 60 hours per week for 12 weeks before the onset of cerebro-cardiovascular disease, it is recognized as an occupational disease by the Public Notice of the Ministry of Employment and Labor in Korea. In accordance with the 2021 Labor Statistics of the Korea Labor Institute, a public institution under the Prime Minister, individuals who work less than 36 hours per week are defined as part-time workers. We excluded part-time workers to minimize deviations in evaluating the health effects of long working hours. Based on the above-mentioned standards, the average weekly working hours over the past year were categorized as 36–40 hours, 41–52 hours, 53–60 hours, and >60 hours per week. The shift work schedule was assessed using the following question: “In the past year, during which time of the day did you work the most?” Daytime work was defined as work performed mostly during the day (between 6 a.m. and 6 p.m.), and shift work was defined as work performed during other hours.
- Blood pressure, weight, and height were measured by trained nurses [17]. Obesity was defined as body mass index (BMI) ≥25 kg/m2. Hypertension was defined as a systolic blood pressure ≥140 mmHg, a diastolic blood pressure ≥90 mmHg, a self-reported history of hypertension, or current use of anti-hypertensive medications. Fasting blood measurements included glucose, thyroid-stimulating hormone (TSH), and free thyroxine (fT4). DM was defined as a fasting serum glucose level of ≥126 mg/dL, a self-reported history of DM, or current use of anti-diabetic medications.
- Thyroid function tests were performed routinely since the first visit, regardless of job position or occupation. Serum TSH and fT4 levels were measured by radioimmunoassay using a commercial kit (RIA-gnost® hTSH, fT4, Schering-Cis Bio International, Gif-sur-Yvette, France), with lower detection limits of 0.025 μIU/mL and 0.06 ng/dL, respectively. The normal range was 0.25–5.0 μIU/mL for TSH and 0.93–1.7 ng/dL for fT4. The intra-assay and inter-assay coefficients of variation for quality control specimens were 1.2–5.7% and 2.4–5.4%, respectively, for TSH, and 2.3–4.4% and 2.1–5.7%, respectively, for fT4 [18]. Hypothyroidism was defined as a serum TSH level above the upper reference limit with a normal serum fT4 level (subclinical hypothyroidism) or a serum fT4 level below the lower reference limit (overt hypothyroidism) [10].
- Statistical analysis
- The baseline characteristics of study participants were presented according to the 4 groups of weekly working hours. Descriptive statistics were used to summarize the characteristics of participants categorized by the groups of working hours. The primary endpoint was the development of incident hypothyroidism (subclinical or overt hypothyroidism). Participants were followed-up from the baseline to the endpoint visit or to the last available visit until December 31, 2018, whichever came first. Incidence density was calculated as the number of incident cases divided by person-years of follow-up.
- Hazard ratios (HRs) and 95% confidence intervals (CIs) for incident hypothyroidism were estimated using Cox proportional hazards regression analyses. Initially, only age and sex were adjusted in the crude model. Model 1 was adjusted for age, sex, alcohol intake, and smoking status. To adjust for the potential confounders, model 2 was further adjusted for DM, hypertension, cardiovascular disease, and BMI. Lastly, to adjust for other occupational risk factors, model 3 was further adjusted for shift work. The proportional-hazards assumption was assessed by examining graphs of estimated log (-log) survival and by using the ‘estat phtest’ command based on Schoenfeld residuals; no violation of the assumption was found. To demonstrate the linear trend of incidence, the group number (corresponding to the category of weekly working hours) was used as a continuous variable and examined in each model.
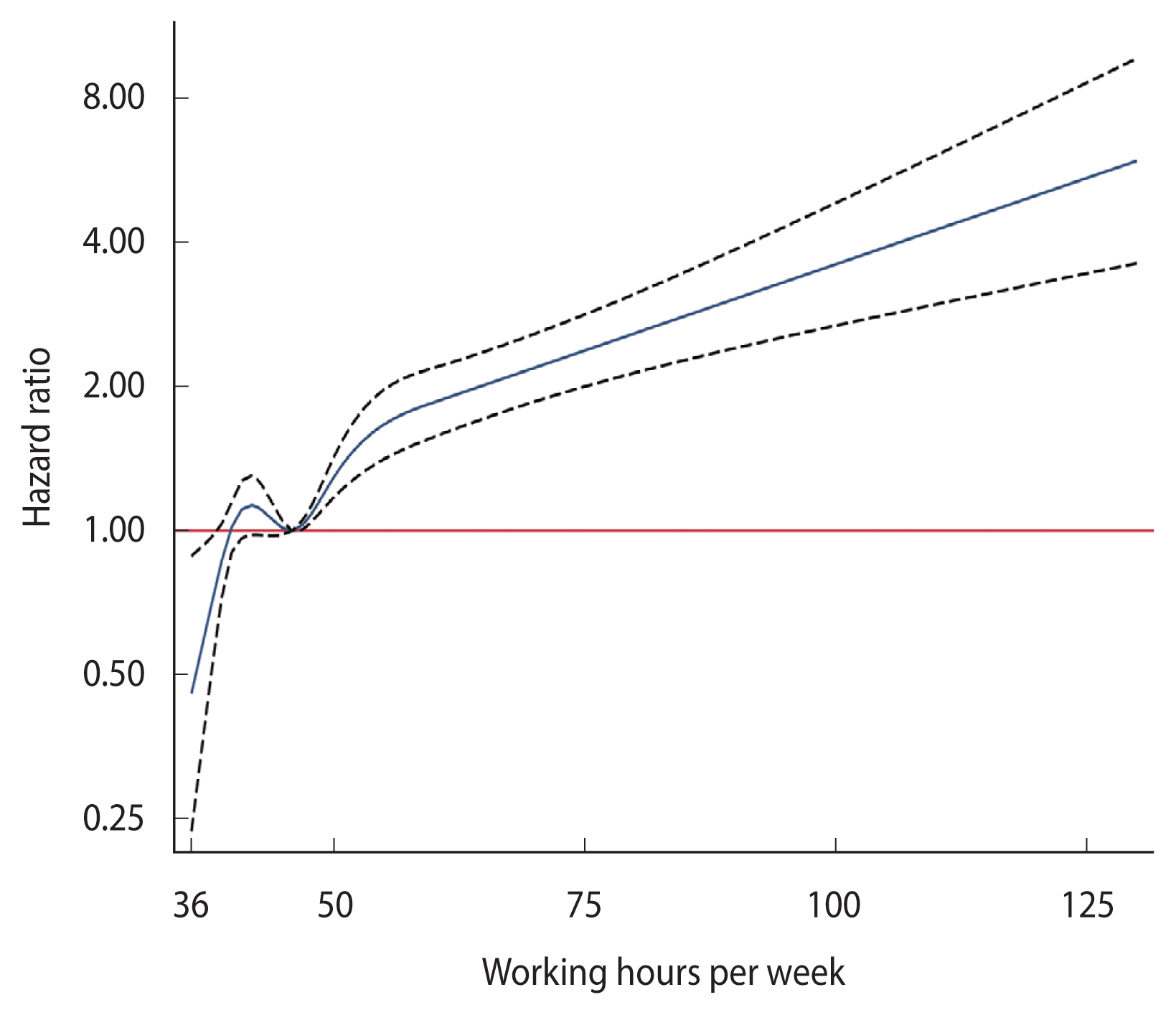
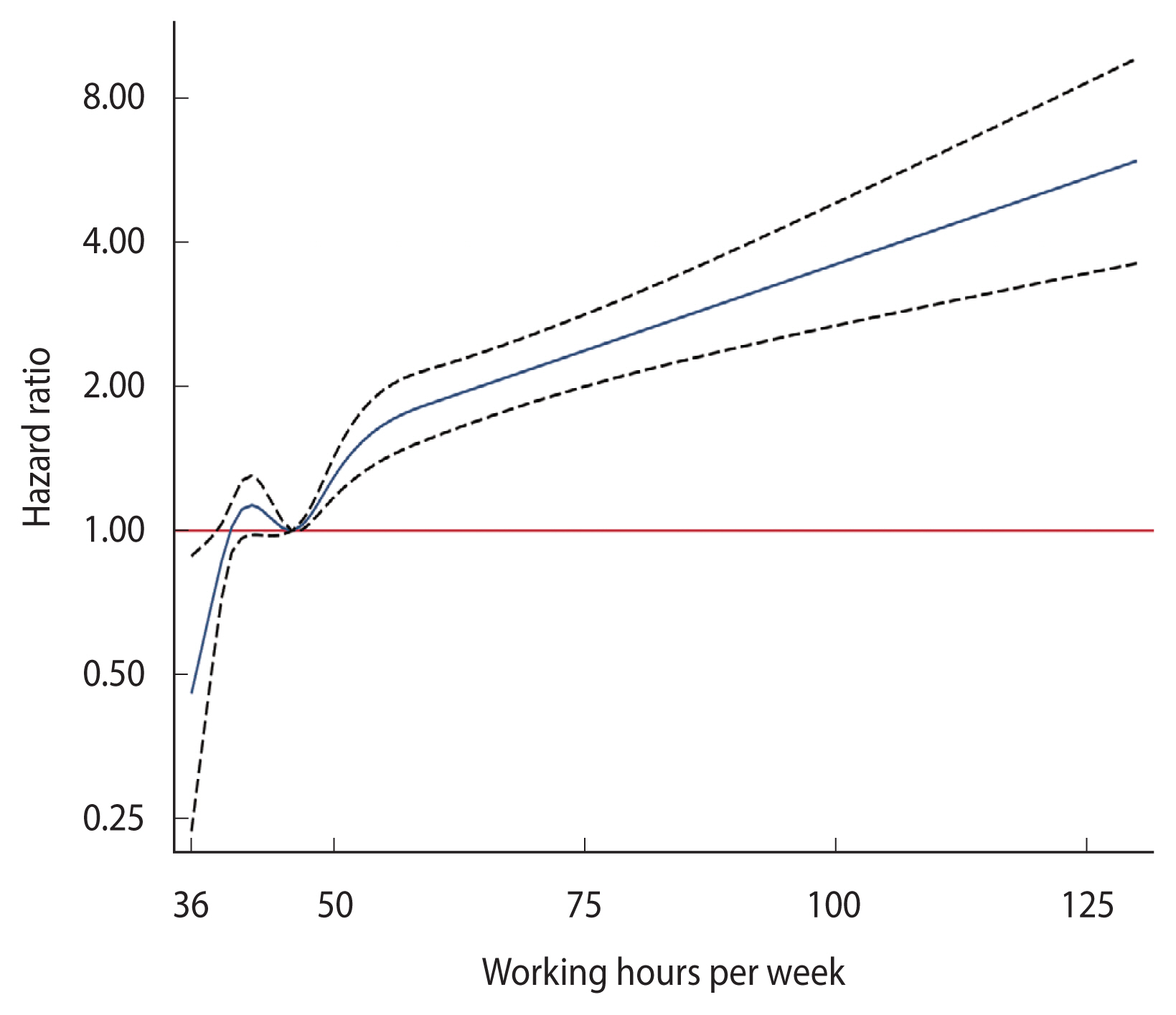
- To further explore a dose-response relationship between long working hours and the risk of hypothyroidism, we conducted 2 dose-response analyses. First, HRs were estimated with 95% CIs associated with a 1-hour increase in weekly working hours used as a continuous variable in the regression models. Second, restricted cubic splines with knots were performed at the 5th, 27.5th, 50th, 72.5th, and 95th percentiles of the baseline distribution of weekly working hours. To explore whether the associations between long working hours and hypothyroidism differed, subgroup analyses were performed by age (<36 vs. ≥36 years, stratified by median age), sex (women vs. men), BMI (<25 vs. ≥25 kg/m2), and shift work schedule (daytime work vs. shift work). Interactions between the groups of working hours and subgroup characteristics were tested using likelihood ratio tests, which compared models with and without
- In a sensitivity analysis to test the robustness of our primary outcomes, we included 90,047 participants whose category of working hours changed during follow-up. Among 135,306 workers, individuals whose category of working hours changed were censored at the time of change. Sequentially, Cox proportional hazards regression analyses and restricted cubic splines with knots were performed in the same way as in the main analysis. Statistical analyses were performed using Stata version 17.0 (StataCorp., College Station, TX, USA). All reported p-values were 2-tailed, and p-values <0.05 were considered statistically significant.
- Ethics statement
- This study was approved by the Institutional Review Board of Kangbuk Samsung Hospital, which waived the requirement for informed consent because we accessed only de-identified data routinely collected as part of health screening examinations (IRB No. KBSMC2022-03-041).
MATERIALS AND METHODS
Interaction terms
- In Table 1, the mean±standard deviation age, serum TSH, and fT4 levels at baseline were 37.6±8.1 years, 2.01±0.97 μIU/mL, and 1.30±0.16 ng/dL, respectively. Weekly working hours were positively associated with male sex, current smoking status, obesity, BMI, systolic blood pressure, diastolic blood pressure, glucose, and fT4 at baseline, and negatively associated with age, hypertension, DM, cardiovascular disease, TSH, and daytime work at baseline.
- The association between weekly working hours and the risk of incident hypothyroidism is shown in Table 2. In a total of 45,259 participants, there were 2,914 incident cases of hypothyroidism (incidence density, 2.11/102 person-years) over 138,261.7 person-years of follow-up (median follow-up, 2.6 years; interquartile range, 1.9–4.2). All models showed a significantly higher risk of hypothyroidism in all groups that worked more than the reference group (working 36–40 hours per week). In model 3, even after introducing all potential confounders considered in the study, the multivariable-adjusted HRs of incident hypothyroidism for working 41–52 hours, 52–60 hours, and >60 hours compared with working 36–40 hours were 1.13 (95% CI, 1.03 to 1.24), 2.53 (95% CI, 2.17 to 2.95), and 2.57 (95% CI, 2.09 to 3.15), respectively. When weekly working hours were introduced as a continuous variable in regression models, the HR associated with a 1-hour increase in model 3 was 1.02 (95% CI, 1.02 to 1.03). After adjustment in all models, the association remained significant. Increased working hours had a dose-response relationship to the risk of incident hypothyroidism, with a significant trend. Moreover, in the multivariable-adjusted spline regression model, there was a significant dose-response relationship between weekly working hours and incident hypothyroidism at almost the entire range of working hours (Figure 2).
- In subgroup analyses (Table 3), a significant association between working more than 52 hours per week and incident hypothyroidism compared with working 36–40 hours per week was consistently shown among participants in all clinically relevant subgroups. However, the association was significantly stronger among participants ≥36 years of age, men, and daytime workers (p for interaction <0.05).
- In the sensitivity analysis (Supplementary Material 1), when Cox proportional hazards regression analyses were performed for 135,306 participants, including workers whose category of working hours changed during follow-up, a significant association between working more than 52 hours per week at baseline and incident hypothyroidism compared with working 36–40 hours per week was observed in all models. Furthermore, a significant association between a 1-hour increase in weekly working hours and incident hypothyroidism was shown. In the multivariable-adjusted spline regression model (Supplementary Material 2), a significant and approximately linear dose-response relationship was found between weekly working hours at baseline with incident hypothyroidism across the full range of working hours, except for 40–50 hours.
RESULTS
- In the present study wherein the participants had euthyroidism with no thyroid disease at baseline, the results demonstrated that working long hours was associated with the development of hypothyroidism in a dose-response manner. Specifically, our large-scale cohort study showed that regularly working more than 52 hours per week was significantly associated with more than a 2-fold higher risk of incident hypothyroidism compared with regularly working 36–40 hours per week. In addition, the association remained significant even after stratification into predetermined subgroups. When we included workers whose weekly working hours fluctuated, the association was slightly attenuated but still significant. Unlike the previous study by Lee et al. [10], our results could evaluate the temporal effect of long-term exposure to consistent overwork.
- To our knowledge, the underlying mechanisms by which long working hours affect the development of hypothyroidism are unknown. Several epidemiological studies investigating the effects of long working hours on health have suggested that the chronic stress response caused by long working hours may play an important role in the biological mechanism [6,19,20]. It is known that long working hours can cause work-related stress such as job strain [3,21]. In turn, chronic psychosocial stress activates the sympathetic nervous system by the hypothalamic-pituitary-adrenal (HPA) axis, stimulates the release of stress hormones such as cortisol, and triggers chronic low-grade inflammation by proinflammatory cytokines [22,23]. As the HPA axis continues to be activated because of chronic stress, HPA axis dysfunction may occur, inducing hypothyroidism by an imbalance of thyroid hormones [24]. In rodent models, repetitive stress triggers the release of cortisol, which suppresses the hypothalamic-pituitary-thyroid (HPT) axis and decreases the peripheral TSH level and thyroid hormone levels [25,26]. A recent epidemiological study by Walter et al. [27] reported a correlation between cortisol and subclinical hypothyroidism. In addition, stress can cause Hashimoto’s thyroiditis by affecting the immune system through the neuroendocrine system (sympathoadrenal and HPA axis) [28]. Posttraumatic stress disorder was found to show a particularly high risk of hypothyroidism, which is explained by inflammatory responses, dysregulation of the HPT axis, and accelerated immune cell aging [29].
- As well as biological mechanisms, negative health behaviors, such as obesity, prolonged sedentary time, and physical inactivity, have been suggested as additional mechanisms for the negative health effect of long working hours [3,6]. First, because long working hours are related to obesity and metabolic syndrome [3,9], these conditions may lead to hypothyroidism [30,31]. Notwithstanding such relevance, our results showed a significant association after adjustment for metabolic abnormalities (model 2 in Table 2) and stratification for obesity (Table 3), implying that other mechanisms are still involved. Second, Thorp et al. [32] reported an association between working hours and sedentary time. Prolonged sedentary time at work may also be linked to physical inactivity [6]. In terms of causing changes in circulating thyroid hormone levels according to physical activity and improving thyroid hormone levels in hypothyroidism patients [33,34], it can be hypothesized that hypothyroidism can be caused by physical inactivity [10]. However, since the effect of physical activity on the thyroid is still a matter of debate [35], further studies are required to explain the underlying mechanism.
- Considering the significant HRs for covariates in Table 2, previous studies have demonstrated an association between shift work and subclinical hypothyroidism [15,16], but other studies have reported discordant findings [36]. Consistent with several previous studies, our findings showed that shift workers had a higher risk of hypothyroidism than daytime workers (HR, 1.25; 95% CI, 1.10 to 1.42). The main mechanism underlying the relationship between shift work and increased TSH levels appears to be the effect of circadian rhythm disruption [16]. In terms of cigarette smoking, the present study showed that current smoking might have been a protective factor against hypothyroidism (HR, 0.81, 95% CI, 0.73 to 0.90). In keeping with these results, previous studies illustrated that the prevalence of hypothyroidism was significantly lower in current smokers than in non-smokers, indicating that smoking is negatively associated with hypothyroidism [12]. Furthermore, DM was also shown in our results as a protective factor against hypothyroidism (HR, 0.78; 95% CI, 0.62 to 0.98). Regarding treatment for DM, metformin has the effect of lowering TSH levels in DM patients with hypothyroidism or TSH levels in upper normal limits, or who are euthyroid and thyroid peroxidase antibody-positive [37,38]. However, in our study, DM patients who were treated with metformin were not separated from DM patients in general, and there were no data on thyroid peroxidase antibody status. Therefore, further studies are needed to concretely identify the relationship between DM and hypothyroidism.
- In subgroup analyses, the association between long working hours and incident hypothyroidism was stronger in older participants and men. It is well-known that old age is a risk factor for hypothyroidism, as serum TSH levels gradually increase with age. The most common reason for hypothyroidism among otherwise healthy elderly individuals is autoimmune thyroiditis [14]. Moreover, with advancing age, hypothalamic dysfunction leads to a realignment of the HPA axis, followed by a decrease in TSH circadian modulation [39]. As long working hours increase stress, the progression of autoimmune thyroiditis and HPA axis dysfunction can be accelerated. Accordingly, it can be inferred that older individuals were more vulnerable to the risk of hypothyroidism with long working hours. However, although shift workers showed a higher risk of hypothyroidism, the risk of long working hours was attenuated among shift workers compared to daytime workers. This may be because shift workers who worked relatively short hours had a high risk of hypothyroidism, and shift workers who worked long hours could have been subject to the healthy worker effect. Therefore, further studies need to be conducted among shift workers.
- It is generally known that women are at higher risk of hypothyroidism [14]. This was supported by the present study results (HR, 1.73; 95% CI, 1.57 to 1.91). However, although our study found that long working hours significantly increased the risk of incident hypothyroidism in both men and women, the risk was 3.06-fold higher in men who worked more than 60 hours than in those who worked 36–40 hours, and their risk was significantly higher than that of women (p for interaction=0.009). An explanation for the finding that the risk of long working hours for hypothyroidism was lower for women than for men may be that the reference group of women for working hours was at an elevated risk of hypothyroidism compared to the reference group of men. Additionally, a study by Loosemore & Waters [40] revealed that male workers in the construction industry experienced more stress than women in relation to risk-taking, disciplinary matters, implications of mistakes, redundancy, and career progression. When employees are at high risk of losing their job or threatened with disciplinary action, it is mandatory rather than voluntary for such workers to work long hours [41]. Another study by Rivera-Torres et al. [42] reported that male workers were strongly stressed by quantitative demands, while female workers perceived pressure from qualitative demands (intellectually or emotionally demanding jobs). In this regard, men may be more vulnerable to work-related stress caused by long working hours than women, which might lead to a higher effect of long working hours on hypothyroidism.
- Several limitations of the present study need to be considered. First, weekly working hours and several covariates were collected by self-administered questionnaires. The possibility of measurement errors occurring in these variables could not be excluded. However, since there was no disadvantage or benefit to the examinees based on the measured values of these variables, there was no reason to overreport or underreport with a specific intention. Thus, our findings would not be affected by any significant differential misclassification. Second, to clearly identify the health effects of long working hours, we excluded those with a fluctuating category of working hours, which might have caused selection bias. However, a significant association between long working hours and the development of hypothyroidism was observed even when a sensitivity analysis was performed using 135,306 potential participants, including workers whose category of working hours changed during follow-up. Hence, the bias would not have a significant effect on our study. Third, since International Classification of Diseases, 10th revision codes could not be used in our study, the incidence of hypothyroidism was determined by using thyroid function tests. There was a questionnaire about the history of any thyroid disease (not specifying hypothyroidism) at baseline. Therefore, we could exclude all thyroid diseases, including hypothyroidism, at baseline. Since people without any thyroid disease were included when selecting the baseline population, it was assumed that hypothyroidism was first diagnosed through the thyroid function test. Fourth, the effect of interval censoring could not be ignored. However, in our study, the average health check-up interval was the same between workers who worked over 52 hours per week and workers who worked less than 52 hours (1.8 vs. 1.8 years). Therefore, differences in the likelihood of detecting hypothyroidism due to long working hours are unlikely to have affected our study results. Fifth, since thyroid function tests were not remeasured 6 months to 1 year after the first measurement, temporary thyroid dysfunction and secondary dysfunction could not be completely ruled out. Moreover, our primary outcomes included subclinical hypothyroidism, as well as overt hypothyroidism, and the age-specific references of thyroid function tests for hypothyroidism were not used. Thus, the incidence density of hypothyroidism in our study would be higher than that in the general population. Sixth, thyroid peroxidase antibody, iodine diet, type of worker (e.g., blue-collar vs. white-collar), occupational stress, and other lifestyle variables were not evaluated in this study. Studying these factors in further research may contribute to elucidating the mechanisms underlying our results. According to the Occupational Safety and Health Act of Korea, a business owner should provide a general health check-up to office workers (white-collar) biennially and to non-office workers annually. When subgroup analysis was performed according to the average health check-up interval (Supplementary Material 3), the risk of hypothyroidism was higher when annual health check-ups were received. This could have been due to exposure to various hazardous substances in blue-collar occupations [43,44]. However, if workers do not receive a health check-up, it can be carried over to the next year, and it is possible to receive an examination at another hospital. Therefore, we could not classify workers as blue-collar or white-collar based on the interval between check-ups. Meanwhile, the extent to which a potential unmeasured confounder negated the observed association between long working hours and hypothyroidism can be assessed by calculating the E-value [45]. In model 3, the measured E-value for working more than 60 hours per week was 4.58 (95% CI, 3.60 to 5.75), suggesting that the observed HR of 2.57 could be explained away by an unmeasured confounder that was associated with both our exposure and outcome by an HR of 4.58-fold each, above and beyond the measured confounders, but weaker confounding could not do so; furthermore, the 95% CI could be shifted to include the null by an unmeasured confounder that was associated with both our exposure and outcome by an HR of 3.60-fold each, above and beyond the measured confounders, but weaker confounding could not do so [45]. The E-value in the present study indicates the robustness of our main findings to unmeasured confounding. Lastly, the participants were young and middle-aged Koreans in relatively good health. Accordingly, our results may not be generalizable to other populations differing in terms of age, race, and ethnicity.
- Notwithstanding the abovementioned limitations, this study has several notable strengths. To the best of our knowledge, this is the first longitudinal study with a large-scale sample size, well-designed cohort, and standardized data to demonstrate the temporal association between long working hours and the development of hypothyroidism. Moreover, by examining a fixed exposure through repeated measurements of working hours, the study examined the effect of long working hours more clearly than before. In this study, only subjects with no change in the category working hours were included to compensate for the inaccuracy of self-questionnaires and to accurately estimate risk by selecting only individuals with constant exposure for reliable survival analysis. However, since the healthy worker effect could have been applicable to those whose working hours did not change, the actual effect might have been underestimated. Therefore, the actual risk might be higher than the results of this study. Lastly, the study was based on a relatively young and middle-aged healthy population, implying less susceptibility to survivor bias from comorbidities.
- In conclusion, our large-scale cohort study demonstrated the association between long working hours and the incidence of hypothyroidism, with a dose-response relationship. As the impacts of long working hours continue to be revealed, more attention should be paid to the health of overworked workers.
DISCUSSION
SUPPLEMENTARY MATERIALS
ACKNOWLEDGEMENTS
-
DATA AVAILABILITY
The data are not available to be shared publicly, because we do not have permission from the institutional review board to distribute the data. However, data can be available from the Kangbuk Samsung Health Study upon reasonable request, whose authors may be contacted through the corresponding author of this manuscript.
-
CONFLICT OF INTEREST
The authors have no conflicts of interest to declare for this study.
-
FUNDING
None.
-
AUTHOR CONTRIBUTIONS
Conceptualization: Lee Y. Formal analysis: Lee Y, Lee W, Kim HR. Funding acquisition: None. Methodology: Lee Y, Kim HR. Writing – original draft: Lee Y. Writing – review & editing: Lee Y, Lee W, Kim HR.
NOTES
| Characteristics | Overall |
Weekly working hours |
p-value for trend | |||
|---|---|---|---|---|---|---|
| 36-40 | 41-52 | 53-60 | >60 | |||
| Total (n) | 45,259 | 15,139 | 26,327 | 2,545 | 1,248 | |
| Age (yr) | 37.6±8.1 | 40.6±8.9 | 36.0±7.1 | 37.4±7.6 | 37.1±8.5 | <0.001 |
| Men | 69.8 | 52.4 | 78.0 | 82.2 | 82.6 | <0.001 |
| Current smoker | 22.5 | 19.0 | 22.9 | 32.3 | 35.5 | <0.001 |
| Alcohol heavy intake1 | 17.0 | 17.8 | 15.9 | 21.0 | 22.0 | 0.419 |
| Hypertension | 11.3 | 13.0 | 10.2 | 13.4 | 10.6 | <0.001 |
| Diabetes mellitus | 3.6 | 5.0 | 2.8 | 3.4 | 3.8 | <0.001 |
| Cardiovascular disease | 1.0 | 1.5 | 0.8 | 0.9 | 1.4 | 0.003 |
| Obesity2 | 31.7 | 27.7 | 32.9 | 38.6 | 38.5 | <0.001 |
| BMI (kg/m2) | 23.7±3.3 | 23.2±3.3 | 23.8±3.3 | 24.3±3.4 | 24.4±3.5 | <0.001 |
| Systolic BP (mmHg) | 109.5±12.7 | 107.7±13.4 | 110.2±12.3 | 111.4±12.5 | 111.3±12.3 | <0.001 |
| Diastolic BP (mmHg) | 70.8±10.1 | 70.2±10.6 | 71.1±9.8 | 71.9±10.1 | 71.2±9.6 | <0.001 |
| Glucose (mg/dL) | 93 (88-99) | 93 (88-100) | 93 (88-99) | 94 (88-99) | 94 (89-100) | 0.001 |
| TSH (μIU/mL) | 2.01±0.97 | 2.01±0.97 | 2.01±0.97 | 1.97±0.98 | 1.98±0.99 | 0.045 |
| free T4 (ng/dL) | 1.30±0.16 | 1.27±0.15 | 1.32±0.15 | 1.31±0.16 | 1.30±0.16 | <0.001 |
| Daytime work3 | 89.9 | 91.8 | 89.5 | 88.7 | 76.5 | <0.001 |
Values are presented as mean±standard deviation, percentage, or median (interquartile range).
BMI, body mass index; BP, blood pressure; TSH, thyroid-stimulating hormone.
1 Women: ≥20 g/day, men: ≥30 g/day.
2 BMI ≥25kg/m2.
3 Participants who answered “I work mostly during the day (between 6 a.m. and 6 p.m.)”.
| Variables | PY | Incident cases | Incidence density (per 102 PY) (95% CI) | Age- and sex-adjusted |
Multivariable-adjusted1 |
|||
|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | ||||||
| Weekly working hours | ||||||||
| 36-40 | 46,576.5 | 1,084 | 2.32 (2.19, 2.47) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | |
| 41-52 | 82,653.6 | 1,484 | 1.80 (1.71, 1.89) | 1.10 (1.01, 1.20) | 1.12 (1.02, 1.22) | 1.12 (1.02, 1.23) | 1.13 (1.03, 1.24) | |
| 53-60 | 5,992.5 | 228 | 3.80 (3.34, 4.33) | 2.44 (2.11, 2.83) | 2.50 (2.15, 2.91) | 2.51 (2.15, 2.92) | 2.53 (2.17, 2.95) | |
| >60 | 3,039.1 | 118 | 3.88 (3.24, 4.65) | 2.42 (1.99, 2.93) | 2.57 (2.10, 3.14) | 2.56 (2.09, 3.12) | 2.57 (2.09, 3.15) | |
| Per 1 hour | 1.02 (1.02, 1.03) | 1.02 (1.02, 1.03) | 1.02 (1.02, 1.03) | 1.02 (1.02, 1.03) | ||||
| p for trend | <0.001 | <0.001 | <0.001 | <0.001 | ||||
| Age | 1.04 (1.03, 1.04) | 1.04 (1.03, 1.05) | 1.04 (1.04, 1.05) | 1.04 (1.04, 1.05) | ||||
| Sex | ||||||||
| Men | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | ||||
| Women | 1.81 (1.67, 1.97) | 1.71 (1.56, 1.88) | 1.75 (1.58, 1.93) | 1.73 (1.57, 1.91) | ||||
| Alcohol intake | ||||||||
| Not heavy drinking | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | |||||
| Heavy drinking | 1.05 (0.95, 1.17) | 1.05 (0.95, 1.17) | 1.05 (0.94, 1.17) | |||||
| Smoking status | ||||||||
| Not current smoker | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | |||||
| Current smoker | 0.82 (0.74, 0.91) | 0.82 (0.74, 0.91) | 0.81 (0.73, 0.90) | |||||
| DM | 0.79 (0.63, 0.98) | 0.78 (0.62, 0.98) | ||||||
| Hypertension | 0.98 (0.86, 1.12) | 0.97 (0.85, 1.10) | ||||||
| Cardiovascular disease | 1.05 (0.73, 1.51) | 1.01 (0.70, 1.46) | ||||||
| BMI | 1.01 (1.00, 1.02) | 1.01 (0.99, 1.02) | ||||||
| Shift work schedule | ||||||||
| Daytime work | 1.00 (reference) | |||||||
| Shift work | 1.25 (1.10, 1.42) | |||||||
Values are presented as hazard ratio (95% CI).
PY, person-years; CI, confidence interval; DM, diabetes mellitus; BMI, body mass index.
1 Estimated from Cox proportional hazard models; Model 1 was adjusted for age, sex, alcohol intake, and smoking status; Model 2: model 1 plus adjustment for hypertension, DM, cardiovascular disease, and BMI; Model 3: model 2 plus adjustment for shift work.
- 1. Bannai A, Tamakoshi A. The association between long working hours and health: a systematic review of epidemiological evidence. Scand J Work Environ Health 2014;40:5-18.ArticlePubMed
- 2. Isahak M, Loh MY, Susilowati IH, Kaewboonchoo O, Harncharoen K, Mohd Amin N, et al. The association of workplace exposures on quality of life in small and medium enterprises workers: a cross-sectional study in four ASEAN countries. Asia Pac J Public Health 2017;29:315-327.ArticlePubMedPDF
- 3. Wong K, Chan AH, Ngan SC. The effect of long working hours and overtime on occupational health: a meta-analysis of evidence from 1998 to 2018. Int J Environ Res Public Health 2019;16:2102.ArticlePubMedPMC
- 4. Lee DW, Lee J, Kim HR, Kang MY. Association of long working hours and health-related productivity loss, and its differential impact by income level: a cross-sectional study of the Korean workers. J Occup Health 2020;62:e12190.ArticlePubMedPMCPDF
- 5. Organisation for Economic Cooperation and Development. Hours worked. [cited 2021 Nov 7]. Available from: https://data.oecd.org/emp/hours-worked.htm .
- 6. Kivimäki M, Jokela M, Nyberg ST, Singh-Manoux A, Fransson EI, Alfredsson L, et al. Long working hours and risk of coronary heart disease and stroke: a systematic review and meta-analysis of published and unpublished data for 603,838 individuals. Lancet 2015;386:1739-1746.ArticlePubMed
- 7. Trudel X, Brisson C, Gilbert-Ouimet M, Vézina M, Talbot D, Milot A. Long working hours and the prevalence of masked and sustained hypertension. Hypertension 2020;75:532-538.ArticlePubMed
- 8. Kivimäki M, Virtanen M, Kawachi I, Nyberg ST, Alfredsson L, Batty GD, et al. Long working hours, socioeconomic status, and the risk of incident type 2 diabetes: a meta-analysis of published and unpublished data from 222 120 individuals. Lancet Diabetes Endocrinol 2015;3:27-34.ArticlePubMedPMC
- 9. Virtanen M, Jokela M, Lallukka T, Magnusson Hanson L, Pentti J, Nyberg ST, et al. Long working hours and change in body weight: analysis of individual-participant data from 19 cohort studies. Int J Obes (Lond) 2020;44:1368-1375.ArticlePubMedPDF
- 10. Lee YK, Lee DE, Hwangbo Y, Lee YJ, Kim HC, Lee EK. Long work hours are associated with hypothyroidism: a cross-sectional study with population-representative data. Thyroid 2020;30:1432-1439.ArticlePubMed
- 11. Kim WG, Kim WB, Woo G, Kim H, Cho Y, Kim TY, et al. Thyroid stimulating hormone reference range and prevalence of thyroid dysfunction in the Korean population: Korea National Health and Nutrition Examination Survey 2013 to 2015. Endocrinol Metab (Seoul) 2017;32:106-114.ArticlePubMedPMCPDF
- 12. Taylor PN, Albrecht D, Scholz A, Gutierrez-Buey G, Lazarus JH, Dayan CM, et al. Global epidemiology of hyperthyroidism and hypothyroidism. Nat Rev Endocrinol 2018;14:301-316.ArticlePubMedPDF
- 13. Biondi B, Cappola AR, Cooper DS. Subclinical hypothyroidism: a review. JAMA 2019;322:153-160.ArticlePubMed
- 14. Yoo WS, Chung HK. Subclinical hypothyroidism: prevalence, health impact, and treatment landscape. Endocrinol Metab (Seoul) 2021;36:500-513.ArticlePubMedPMC
- 15. Coppeta L, Di Giampaolo L, Rizza S, Balbi O, Baldi S, Pietroiusti A, et al. Relationship between the night shift work and thyroid disorders: a systematic review and meta-analysis. Endocr Regul 2020;54:64-70.ArticlePubMed
- 16. Leso V, Vetrani I, Sicignano A, Romano R, Iavicoli I. The impact of shift-work and night shift-work on thyroid: a systematic review. Int J Environ Res Public Health 2020;17:1527.ArticlePubMedPMC
- 17. Chang Y, Jung HS, Cho J, Zhang Y, Yun KE, Lazo M, et al. Metabolically healthy obesity and the development of nonalcoholic fatty liver disease. Am J Gastroenterol 2016;111:1133-1140.ArticlePubMedPDF
- 18. Zhang Y, Chang Y, Ryu S, Cho J, Lee WY, Rhee EJ, et al. Thyroid hormone levels and incident chronic kidney disease in euthyroid individuals: the Kangbuk Samsung Health Study. Int J Epidemiol 2014;43:1624-1632.ArticlePubMed
- 19. Descatha A, Sembajwe G, Pega F, Ujita Y, Baer M, Boccuni F, et al. The effect of exposure to long working hours on stroke: a systematic review and meta-analysis from the WHO/ILO Joint Estimates of the Work-related Burden of Disease and Injury. Environ Int 2020;142:105746.ArticlePubMed
- 20. Lee DW, Lee J, Kim HR, Jun KY, Kang MY. Long work hours and decreased glomerular filtration rate in the Korean working population. Occup Environ Med 2020;77:699-705.ArticlePubMed
- 21. Lee K, Suh C, Kim JE, Park JO. The impact of long working hours on psychosocial stress response among white-collar workers. Ind Health 2017;55:46-53.ArticlePubMedPMC
- 22. Tsigos C, Chrousos GP. Hypothalamic-pituitary-adrenal axis, neuroendocrine factors and stress. J Psychosom Res 2002;53:865-871.ArticlePubMed
- 23. Almadi T, Cathers I, Chow CM. Associations among work-related stress, cortisol, inflammation, and metabolic syndrome. Psychophysiology 2013;50:821-830.ArticlePubMed
- 24. Snipes DE. Lifestyle factors contributing to HPA-axis activation and chronic illness in Americans. Arch Neurol Neurosci 2019;5:000608.Article
- 25. Helmreich DL, Parfitt DB, Lu XY, Akil H, Watson SJ. Relation between the hypothalamic-pituitary-thyroid (HPT) axis and the hypothalamic-pituitary-adrenal (HPA) axis during repeated stress. Neuroendocrinology 2005;81:183-192.ArticlePubMedPDF
- 26. Helmreich DL, Tylee D. Thyroid hormone regulation by stress and behavioral differences in adult male rats. Horm Behav 2011;60:284-291.ArticlePubMedPMC
- 27. Walter KN, Corwin EJ, Ulbrecht J, Demers LM, Bennett JM, Whetzel CA, et al. Elevated thyroid stimulating hormone is associated with elevated cortisol in healthy young men and women. Thyroid Res 2012;5:13.ArticlePubMedPMCPDF
- 28. Mizokami T, Wu Li A, El-Kaissi S, Wall JR. Stress and thyroid autoimmunity. Thyroid 2004;14:1047-1055.ArticlePubMed
- 29. Jung SJ, Kang JH, Roberts AL, Nishimi K, Chen Q, Sumner JA, et al. Posttraumatic stress disorder and incidence of thyroid dysfunction in women. Psychol Med 2019;49:2551-2560.ArticlePubMed
- 30. Song RH, Wang B, Yao QM, Li Q, Jia X, Zhang JA. The impact of obesity on thyroid autoimmunity and dysfunction: a systematic review and meta-analysis. Front Immunol 2019;10:2349.ArticlePubMedPMC
- 31. Wang Y, Lin H, Li Q, Guan L, Zhao M, Zhong F, et al. Association between different obesity phenotypes and hypothyroidism: a study based on a longitudinal health management cohort. Endocrine 2021;72:688-698.ArticlePubMedPMCPDF
- 32. Thorp AA, Healy GN, Winkler E, Clark BK, Gardiner PA, Owen N, et al. Prolonged sedentary time and physical activity in workplace and non-work contexts: a cross-sectional study of office, customer service and call centre employees. Int J Behav Nutr Phys Act 2012;9:128.ArticlePubMedPMCPDF
- 33. Ciloglu F, Peker I, Pehlivan A, Karacabey K, Ilhan N, Saygin O, et al. Exercise intensity and its effects on thyroid hormones. Neuro Endocrinol Lett 2005;26:830-834.PubMed
- 34. Bansal A, Kaushik A, Singh CM, Sharma V, Singh H. The effect of regular physical exercise on the thyroid function of treated hypothyroid patients: an interventional study at a tertiary care center in Bastar region of India. Arch Med Health Sci 2015;3:244-246.Article
- 35. Roa Dueñas OH, Koolhaas C, Voortman T, Franco OH, Ikram MA, Peeters RP, et al. Thyroid function and physical activity: a population-based cohort study. Thyroid 2021;31:870-875.ArticlePubMed
- 36. Chen HH, Chiu HH, Yeh TL, Lin CM, Huang HY, Wu SL. The relationship between night shift work and the risk of abnormal thyroid-stimulating hormone: a hospital-based nine-year follow-up retrospective cohort study in Taiwan. Saf Health Work 2021;12:390-395.ArticlePubMedPMC
- 37. Cannarella R, Condorelli RA, Barbagallo F, Aversa A, Calogero AE, La Vignera S. TSH lowering effects of metformin: a possible mechanism of action. J Endocrinol Invest 2021;44:1547-1550.ArticlePubMedPMCPDF
- 38. Dimic D, Golubovic MV, Radenkovic S, Radojkovic D, Pesic M. The effect of metformin on TSH levels in euthyroid and hypothyroid newly diagnosed diabetes mellitus type 2 patients. Bratisl Lek List 2016;117:433-435.Article
- 39. Duntas LH. Thyroid function in aging: a discerning approach. Rejuvenation Res 2018;21:22-28.ArticlePubMed
- 40. Loosemore M, Waters T. Gender differences in occupational stress among professionals in the construction industry. J Manag Eng 2004;20:126-132.Article
- 41. Dembe AE, Erickson JB, Delbos RG, Banks SM. The impact of overtime and long work hours on occupational injuries and illnesses: new evidence from the United States. Occup Environ Med 2005;62:588-597.ArticlePubMedPMC
- 42. Rivera-Torres P, Araque-Padilla RA, Montero-Simó MJ. Job stress across gender: the importance of emotional and intellectual demands and social support in women. Int J Environ Res Public Health 2013;10:375-389.ArticlePubMedPMC
- 43. Boas M, Feldt-Rasmussen U, Skakkebaek NE, Main KM. Environmental chemicals and thyroid function. Eur J Endocrinol 2006;154:599-611.ArticlePubMed
- 44. Huang CC, Ho CH, Chen YC, Hsu CC, Lin HJ, Su SB, et al. Increased risk for hypothyroidism associated with carbon monoxide poisoning: a nationwide population-based cohort study. Sci Rep 2019;9:16512.ArticlePubMedPMCPDF
- 45. VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med 2017;167:268-274.ArticlePubMed
REFERENCES
Figure & Data
References
Citations

- Association between shift work and the risk of hypothyroidism in adult male workers in Korea: a cohort study
Seonghyeon Kwon, Yesung Lee, Eunhye Seo, Daehoon Kim, Jaehong Lee, Youshik Jeong, Jihoon Kim, Jinsook Jeong, Woncheol Lee
Annals of Occupational and Environmental Medicine.2023;[Epub] CrossRef

 KSE
KSE

 PubReader
PubReader ePub Link
ePub Link Cite
Cite